The policy forum is strategically designed to increase participation from members on critical policy issues that impact physicians and the care of patients.
WHAT HAPPENS NEXT
The policy issues were presented and discussed during the 2024 NDMA Annual Meeting then forwarded to the Council for further vetting. The Council met in November to further review and discuss the comments on each policy issue shared during the policy forum.
The Council acted and passed the policies without further changes.. To learn more about policy development and how it works, check out this guide
|
2024 POLICY FORUM TOPICS |
Recreational Marijuana Ballot Measure
The 2024 ballot measure would allow for the production, processing, and sale of cannabis and the possession and use of various forms of cannabis by individuals who are 21 years of age and older; direct a state entity to regulate and register adult-use cannabis and provide protections for individuals who are 21 years of age or older who use cannabis.
Relevant Information:
- North Dakota voters have twice rejected the legalization of recreational marijuana
- Despite the danger to children, the sale of gummies will be allowed by law. In just five years, the number of small children in the US exposed to cannabis after accidentally eating an edible rose 1,375% in kids under 6, according to an analysis of records from the National Poison Data System.
- Risk for substance use disorder is significantly higher for marijuana users (up to 30%) than alcohol users and is associated with a significantly increased risk of use of other illicit substances.
- Enforcing legalization limitations will add to the burden facing law enforcement.
- The measure prohibits local subdivisions from regulating use.
- Cannabis use and possession should be decriminalized, and civil fines and fees should be eliminated whenever possible. Referral for clinical assessment or educational activities are preferred as alternatives to civil penalties. Penalties disproportionately punish people of limited means.
- States should offer automatic expungement for past minor cannabis-related convictions so that hundreds of thousands of people — disproportionately people of color — do not remain marginalized for prior offenses.
NDMA should oppose the ballot measure. Cannabis use should be discouraged through evidence-based prevention programs. NDMA should advocate for greater decriminalization of cannabis use, and greater access to treatment (geographic, pediatric and adult, and financial) should be improved.
Adopted November 26, 2024
Community Health Worker
The Community Health Worker Task Force, created by the ND 2023 Legislature House Bill 1028, was directed to provide the following to the ND Dept. of Health and Human Services: a data-driven plan for community health workers, including scope of work.
Relevant Information:
- Community Health Worker (CHW) scope of practice is widely variable based on the needs of the community and the talents/capacity of the CHW, including but not limited to screening (paper screens as well as blood sugar checks, blood pressure monitoring, foot screens for the presence of ulcers…things one would expect a patient/family member could be trained to do at home), improving access to care via transportation/care coordination, home visits
- Community Health Worker-supported interventions are especially helpful in underserved populations. They increase the likelihood of obtaining primary care, improve mental health, and reduce the likelihood of multiple 30-day readmissions from 40% to 15.2%.
Proposed Action:
NDMA will monitor and advocate where needed to support the CHW task force. Some options of support may be:
- Scope of practice: monitor administrative rules that reflect the practice of skills that can be reasonably taught to and performed by a typical high school graduate.
- Reimbursement: Community Health Worker funding source, competitive worker payment model, and CHW training program support.
- Program Continuation: Adoption of a succession plan to maintain the program after the mandate has expired.
Adopted November 26, 2024
Behavioral Health Dual Diagnosis Treatment
Patrons of North Dakota struggling with a dual diagnosis of a psychiatric illness and substance abuse have limited access to meaningful treatment. They have less longer-term success rates with sobriety as well as mental health wellbeing given the current healthcare service structure in our great state. While we have various options addressing aspects of the services needed for these patients (i.e. housing, psychiatric treatment, substance abuse rehab) they often are not used conjointly nor are financially feasible given limitations in funding via North Dakota Medicaid (abbr. ND MA), other private insurance companies’ payment structures or due to lack of awareness of these resources via the major care providers and case management teams. Most patients struggling with dual diagnosis are likely without insurance, having lost their insurance, or having applied for/already on ND MA. In addition to the above set of patients, there lies another subset within, those with a dual diagnosis who now lack capacity from the severity of their conditions, albeit chronic brain damage from substance abuse vs severe psychiatric illness, limiting their ability to understand their medical conditions or need for treatment. This population cannot participate in most, if not all, of our current outpatient/residential services as they will need 24/7 care and cannot participate in these services voluntarily. Our state has one place for these patients until they clinically improve: the Jamestown State Hospital. The State Hospital is and has been at capacity for a very long time, recently noting 20+ residents that live there because they are unable to be discharged due to placement barriers plaguing our state.
Relevant Information:
North Dakota faces a serious lack of behavioral health services and professionals for treating persons struggling with illicit substance/alcohol abuse because of or in addition to psychiatric conditions (anxiety, depression/PTSD, schizophrenia etc.) The resources available are not well-known to physicians or to patients. The ND Dept. of Health and Human Services acknowledges the need to continue building on resources.
Proposed Action:
While behavioral health care has become more standardized, services and programs are still fragmented for healthcare professionals seeking solutions for patients’ behavioral health needs. Perhaps this is due to a lack of awareness by healthcare professionals of what programs are available for patients. An attempt to increase awareness is necessary.
NDMA will monitor and advocate where needed to support the ND Dept. of Health and Human Services Behavioral Health Division. NDMA should communicate to its members about the availability of the resources for behavioral health and assist with notifying major healthcare systems of North Dakota.
Support and promote the development of a unifying system to track the use of the abovementioned resources and assist in identifying the availability of resources on our state for healthcare systems (i.e. case managers) to better optimize use of these resources.
Support the development of a state-run nursing facility for long-term residents to transition from the state hospital to an outpatient setting, easing the bottle neck effect of patient’s getting stuck within the state hospital, allowing for better use of resources at the inpatient level.
Adopted November 26, 2024
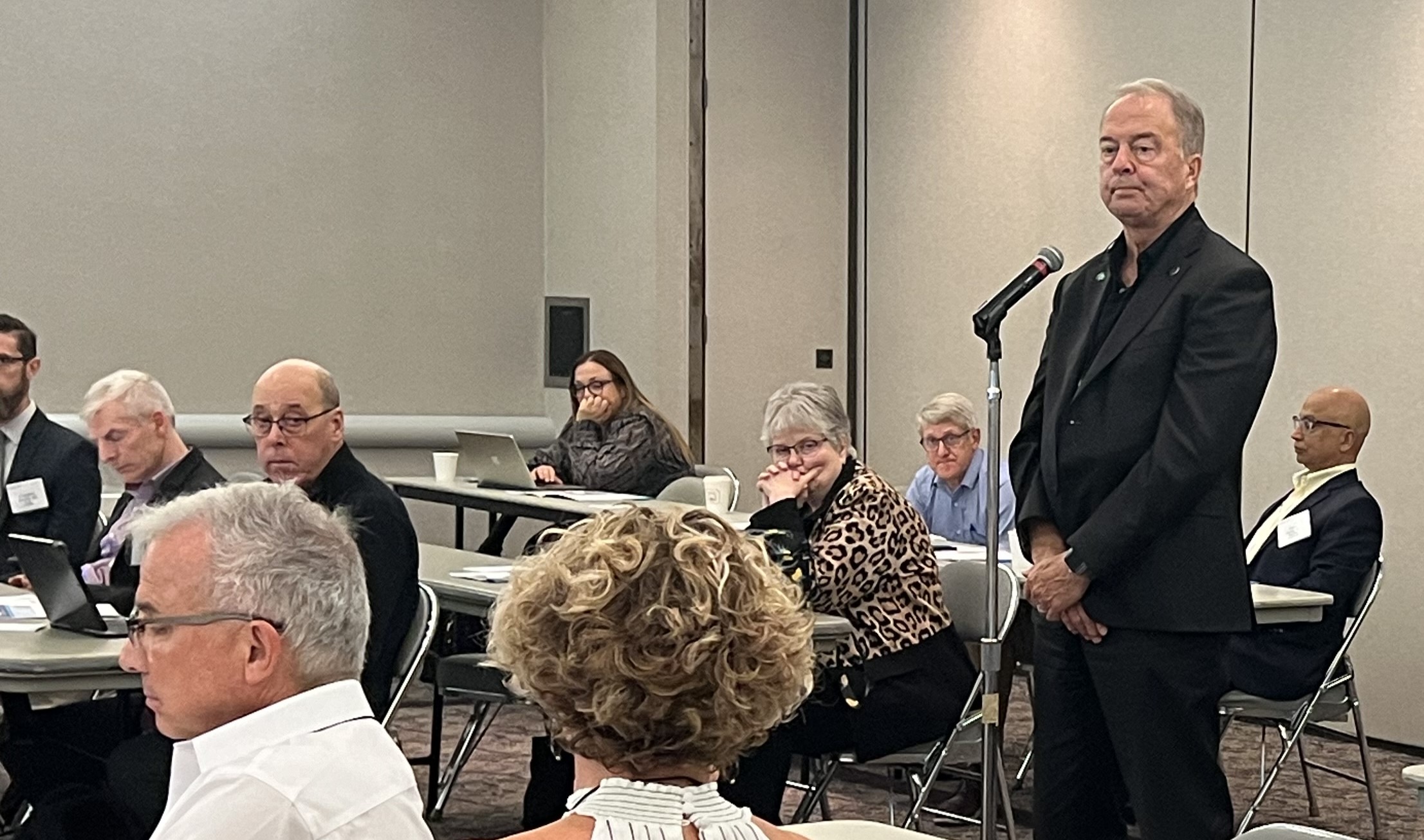
The 2024 Policy Forum discussion included many great debates to assure the ideas presented would contribute to sound policy. Here are a few photos of the event:
 |
||
|
Dr. Erik Heitkamp shares concerns about the need for coordinated care for behavioral health dual-diagnosis patients.
|

The crowd listens intently to each presentation.

|
Dr. Josh Ranum provides insight into several issues and how sound could improve patients’ lives, particularly in rural settings. |
|
|
|